Secondary Iron Overload
*** AWARENESS/ADVOCACY POST ***
This article is written from a patient experience perspective and is *** NOT MEDICAL ADVISE ***. Please use this article to support your Iron Overload investigation and of course, always consult your medical care professional(s).
Background
A common side effect of chemotherapy treatments is low blood counts. In response to low blood counts, Red Blood Cell (RBC) transfusions are a necessary treatment.
A single unit of blood used during a RBC transfusion contains between 200 and 250 milligrams of iron. The body has no normal mechanism for getting rid of any extra iron in the body. To combat this, the body stores extra iron in organs. Long-term storage of iron can damage these organs.
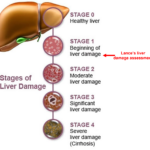
In September of 2020, Lance was clinically diagnosed with Transfusional Hemosiderosis which is the accumulation of iron in the liver and heart but also endocrine organs, in patients who receive or did receive frequent blood transfusions. This diagnosis is also called (Secondary) Iron Overload (IO) and is often mentioned with (Hereditary) Hemochromatosis. Severe IO causes the same symptoms as in Hemochromatosis and can lead to conditions such as: fibrosis/scarring, cirrhosis, diabetes, heart failure, infertility, joint pain, and liver cancer (see Merck Manual link).
There are a ton of articles available in any Internet search. Two articles that we found helpful from a general overview perspective are included here:
Link – Cancer.org: Blood Transfusions for People with Cancer
PDF from Montefiore Medical Center: What is Iron Overload?
Link – Merck Manual: Secondary Iron Overload
How Was Lance’s IO Discovered?
Lance’s IO condition was discovered at a routine “survivorship” check up. The care team included a blood test for Serum Ferritin. It came back high.
Lance was advised to wait a few months and have his Serum Ferritin retested. The reason for this delay and non-concern was that Serum Ferritin can be high for a number of reason, including inflammation from the common cold. After the advised waiting period passed, Lance’s Serum Ferritin was retested and came back high again. These two high blood test result triggered a return visit to his oncology care team to address the issue.
So What’s the Big Deal?
The oncology care team conveyed that their suspicion was that RBC transfusions Lance had during his cancer treatment was the likely the cause of the high Serum Ferritin.
Link – Mayo Clinic: Info on Ferritin Test
At Lance’s 1st return visit to his in-clinic oncology team, they were not really concerned. They were surprised Lance had had as many RBC transfusions that their records indicated (20), but they had seen Serum Ferritin levels many times higher than Lance’s 1171 NG/ML. Their treatment plan – put into action with no other testing or baselines recorded – was to start Therapeutic Phlebotomy sessions and that Lance would “only need 2 or 3 sessions to clear things up.”
Therapeutic Phlebotomies (or blood donations for hemochromatosis patients who can give blood at a blood bank) work via a mechanism that when blood is removed from the body, organs that are storing iron, for example the liver, release iron to assist the body in recovery. An Internet search will not really tell you this… unless you have an advanced medical degree.
The oncology care team was right about the RBC transfusions likely being the cause for the high Serum Ferritin levels but they would (1) be wrong about the number of Therapeutic Phlebotomy sessions that would be needed and (2) that they were overlooking a serious IO condition without knowing all of the facts related to Lance’s case.
What Concerned Us?
While we accepted Lance’s initial diagnosis at face value, there was one thing that was leading us to try and understand more about “where he might be”. That one factor was – Time. The only reason you begin care to reduce the amount of iron on your body is so that the excess iron in your body does not do damage to your end-organs. Our concern centered on the fact it had been five (5) years since Lance’s last blood transfusion.
It turned out our concern was justified.
After three (3) Therapeutic Phlebotomy sessions, Lance was advised he needed to move on to a primary care physician to continue care. Lance’s Serum Ferritin was still high (543 NG/ML) but his oncology care team did not feel like their time was needed in Lance’s care from this point on. This is where we finally were able to step in and demand some level setting on “where Lance was at” and demanded an MRI measuring for iron concentration be performed. Begrudgingly an MRI was ordered. The results stunned everyone:”
From the above MRI statement, Lance’s Liver Iron Concentration (LIC) came back at 13.3 grams which is in the moderate/severe range. It also showed iron concentration in Lance’s spleen and bone marrow. It confirmed the Transfusional Hemosiderosis diagnosis.
Lance’s MRI results were AFTER 3 Therapeutic Phlebotomy sessions
The point made above about being “AFTER 3 Therapeutic Phlebotomy sessions”, is that where Lance was at before the 1st sessions was much worse.
- Calculations put Lance’s LIC at 20 to 23 grams in September of 2020 when his IO condition was initially diagnosed. This is in the severe LIC range, and Lance was in this severe range for five (5) years.
- A 20-year-old liver should have under 1 gram of iron stored in it.
- Lance’s Hepatic Iron Index (HII) was calculated at 11.9
An HII less than 1.0 is consistent with normal iron accumulation. An HII 1.0 through 1.9 is consistent with mild iron accumulation such as in heterozygous hemochromatosis or alcoholic liver disease. An HII greater than 1.9 is consistent with iron overload such as in homozygous hemochromatosis, porphyria cutanea tarda, and cirrhotic liver disease. The HII will decrease with chelation, chronic blood loss, or Phlebotomy.
Link: HII Calculator
Change in Attitude
The results of the MRI stunned the care team. A care plan was put in place with specific goals based on measurable numbers, chelation was added, and additional care team members were brought on board (GI, Cardiologist, adult Oncologist).
The primary “number” in the care plan is to get Lance’s Serum Ferritin below 100 NG/ML and have it stay there for a period of time (months). After some period of time another Abdomen MRI checking for LIC will be performed to see if Lance’s liver is still holding onto a lot of iron. At that time a decision will be made to stop or continue with additional Therapeutic Phlebotomy sessions.
To date Lance has had eleven (11) Therapeutic Phlebotomy sessions and his Serum Ferritin is hanging out in the 150-200 NG/ML range.
We do know the Therapeutic Phlebotomy sessions are working – as measured by the (slowly) lowering of Lance’s Serum Ferritin level and we also had a 2nd Abdomen MRI performed that showed Lance’s LIC at 4.2 grams.
Our Message
If your child is (or has) receiving (received) RBC transfusions during cancer treatment, advocate for complete monitoring and detailed understanding of the impact of these transfusions on their body. Your care team likely is monitoring the key liver, kidney, and heart function indicators, but may not be understanding the whole picture that, in Lance, went hidden and resulted in “life threatening” (care team comment) Liver Iron Concentration (LIC) levels.
If your child is being prescribed Therapeutic Phlebotomy sessions to address an IO diagnosis:
- We strongly advocate that BEFORE the 1st session an Abdomen MRI assessing for LIC and Hepatic Iron Index be performed
- We would also encourage assessing the liver for fatty liver disease and fibrosis/scarring of the liver if any significant amount of time has passed since the child’s last RBC Transfusion
Link: FibroScan Scoring
Lance’s Fibrosis/Scarring FibroScan score was a 6 – which is at the high end of F1. NOTE: Lance’s FibroScan was conducted AFTER nine (9) Therapeutic Plebotomy sessions had already occurred. Your liver can heal, and it is likely Lance’s Fibrosis score would have been significantly higher if it had been tested before the 1st Therapeutic Phlebotomy.
- If significant LIC is found in the liver, we would also encourage a Cardiac MRI assessing for iron concentration and disease
As you do your research
If there is one clear message our research uncovered about Secondary Iron Overload in children (and adults as well), is that nothing is clear.
Unclear messaging we found to be frustrating:
- How many RBC transfusions does it take to become a problem? We’ve seen guidance on 10 units, 20 units and even 40 units being level of concerns.
- We were not medically advised to get a level-set of where Lance was at diagnosis of the IO condition. Treatments started with no understanding of what his LIC level was, or what his HII was, or if any other organs were involved.
- Damage. There are mixed messaging about if Hemosiderosis vs Hemochromostosis storage patterns in the organs lead to damage.
Lance had between 18 and 21 RBC Transfusions (medical records showed different #’s). This is also another mystery – because 20 units of blood would only add 5 grams of iron into Lance’s body. Lance was found to have between 20 and 23 grams of iron on his liver. Where did the other 15 or so grams of iron come from?
We can’t emphasize enough, that at a minimum, before the 1st Therapeutic Phlebotomy session a level-setting Abdomen MRI assessing for LIC and Hepatic Iron Index be performed. If possible, we encourage that a FibroScan be performed as well, especially if there has been some time since the last RBC Transfusion.
Not Medical Advise
As we stated in the beginning this post is being shared to provide ONE patient’s experience. The information on this page is not medical advise and your use of this page is for informational purposes only. Good luck!